Low sodium in your blood can be incredibly dangerous, impacting nerve and muscle function, as well as fluid balance. Acute hyponatremia, when your sodium levels drop suddenly, requires immediate attention. For further ICD-10 coding information, see this resource. This article serves as a clinician’s guide to diagnosing and treating acute hyponatremia effectively, including differentiating between hypovolemic, euvolemic, and hypervolemic types, and emphasizing the crucial differences between managing this urgent situation versus chronic low sodium.
Acute Hyponatremia: A Comprehensive Guide for Clinicians
Acute hyponatremia is a medical emergency demanding swift diagnosis and intervention. Sodium, a vital electrolyte, plays a critical role in nerve and muscle function. This guide helps healthcare professionals and informed individuals understand the complexities of acute hyponatremia. What are the possible complications of neglecting timely treatment for acute hyponatremia?
Understanding Hyponatremia and Its Clinical Significance
Hyponatremia indicates a low concentration of sodium in the blood. “Acute” signifies a rapid onset, distinguishing it from chronic hyponatremia, which develops gradually and requires a different management approach. This sudden drop in sodium can lead to a range of symptoms, from mild confusion to severe neurological complications such as seizures and coma. Identifying the underlying cause is essential, as different etiologies require specific treatment strategies.
- Neuromuscular Function: Sodium is essential for action potential generation and propagation in neurons and muscle cells.
- Fluid Balance: Sodium is a key determinant of extracellular fluid osmolality and plays a central role in regulating body water balance.
- Severity Varies: Symptoms can range from subtle cognitive changes to life-threatening neurological manifestations.
Diagnosing Acute Hyponatremia: A Systematic Approach
Accurate diagnosis of the cause and type of acute hyponatremia is critical for effective treatment. The diagnostic process involves assessing multiple factors:
- Clinical Assessment: Evaluate for symptoms such as confusion, nausea, vomiting, headache, muscle weakness, or seizures, with symptom severity indicating treatment urgency. A thorough neurological examination is essential.
- Laboratory Evaluation: Serum sodium level measurement confirms hyponatremia. A comprehensive metabolic panel (CMP) helps assess other electrolytes, renal function, and glucose levels. Serum osmolality should also be measured to confirm hypotonic hyponatremia.
- Volume Status Assessment: Determining the patient’s volume status (hypovolemic, euvolemic, or hypervolemic) guides treatment strategies. Clinical signs, such as skin turgor, mucous membrane moisture, jugular venous pressure, and presence of edema, are assessed.
Determining the patient’s volume status is pivitol in determining the treatment approach. Hypovolemic hyponatremia results from a loss of both sodium and water, but with a relatively greater sodium loss. Euvolemic hyponatremia indicates a normal fluid balance. Hypervolemic hyponatremia results from an increase in both sodium and water, but with a relatively greater water gain.
Identifying Types of Hyponatremia Based on Volume Status
Understanding the type of hyponatremia, based on the patient’s overall fluid balance, is crucial for guiding treatment. Accurate measurement of urine osmolality and urine sodium levels helps pinpoint the underlying cause.
- Hypovolemic Hyponatremia: Characterized by a decrease in total body water and a greater decrease in total body sodium. Common causes include gastrointestinal losses (vomiting, diarrhea), diuretic use, and adrenal insufficiency. Urine sodium is typically low (<20 mEq/L) in extrarenal losses and high (>20 mEq/L) in renal losses (diuretics, salt-wasting nephropathy).
- Euvolemic Hyponatremia: Characterized by normal total body water with an increase in relation to total body sodium. Common causes include SIADH (Syndrome of Inappropriate Antidiuretic Hormone secretion), hypothyroidism, glucocorticoid deficiency, and polydipsia. Urine osmolality is typically inappropriately high (>100 mOsm/kg) in SIADH.
- Hypervolemic Hyponatremia: Characterized by an increase in both total body water and total body sodium, with a relatively greater increase in total body water. Common causes include heart failure, liver cirrhosis, and nephrotic syndrome. Urine sodium is typically low (<20 mEq/L) as the kidneys attempt to retain sodium.
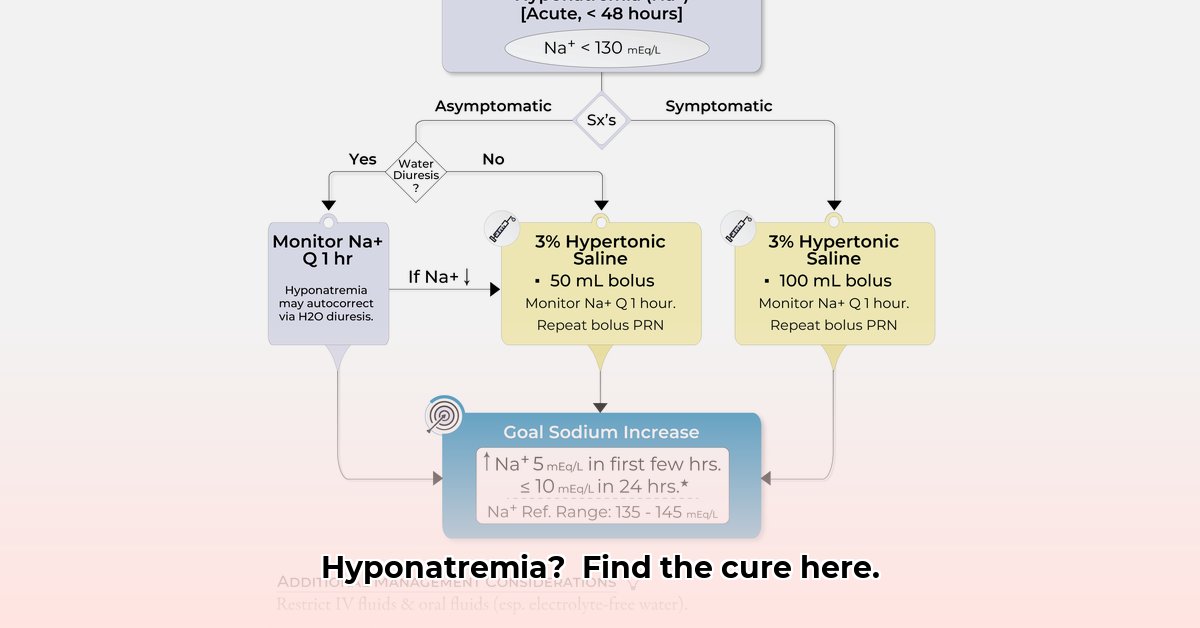
Treating Acute Hyponatremia: A Step-by-Step Approach
Treatment focuses on safely and gradually increasing serum sodium levels while addressing the underlying cause. Rapid sodium drops can cause neurological damage, making timely intervention essential in acute cases. What are alternative treatment options when intravenous access is unobtainable?
Intravenous hypertonic saline (3% NaCl) is the primary treatment for symptomatic acute hyponatremia. This concentrated saline solution increases the serum sodium concentration; however, overly rapid administration can cause osmotic demyelination syndrome (ODS).
Here’s a simplified treatment algorithm:
| Step | Action | Monitoring | Important Considerations |
|---|---|---|---|
| 1. Assessment | Thorough clinical evaluation, including assessment of symptoms, fluid status (hypo-, eu-, hypervolemic), severity. | Continuous monitoring of vital signs (blood pressure, heart rate, respiratory rate), neurological status. | Rapid assessment is crucial to determine appropriate intervention. |
| 2. Bloodwork | Obtain serum sodium levels, serum osmolality, urine osmolality, and urine sodium levels. | Repeat serum sodium measurements every 2-4 hours initially, frequency adjusted based on severity and response to treatment. | Accurate and frequent measurements are essential to monitor treatment efficacy and prevent overcorrection. |
| 3. Treatment | Initiate intravenous hypertonic saline (3% NaCl) infusion. | Monitor serum sodium levels every 1-2 hours during initial correction. | Infusion rate is adjusted based on symptoms, initial sodium level, and ongoing response. Avoid rapid correction to minimize the risk of ODS. |
| 4. Adjustment | Continuously monitor sodium levels and adjust the saline infusion rate accordingly. | Closely observe for improvement or worsening of neurological symptoms. | Slow and steady correction is the goal. Aim for a target increase of 4-6 mEq/L in the first 24 hours. |
| 5. Root Cause | Address the underlying cause of hyponatremia (e.g., dehydration, SIADH). | Ongoing monitoring and management of the underlying condition. May need specialist consultation (nephrology, endocrinology). | Comprehensive management of the underlying cause is critical for long-term resolution. |
Caution: Overly rapid correction can result in ODS (osmotic demyelination syndrome), a severe neurological complication. The target is a carefully managed increase of 4-6 mmol/L in the initial 24 hours, with a maximum of 8 mmol/L in any 24-hour period in patients at high risk for ODS. What are the best practices and potential pitfalls in managing hypertonic saline infusion rates to minimize ODS risk?
Transitioning to Chronic Hyponatremia Management
Chronic hyponatremia requires a more cautious approach focused on identifying and treating the underlying condition. Due to the increased risk of ODS, correction of serum sodium levels should be slower, with increases of 4-8 mmol/L/day, and close monitoring of neurological status.
Case Illustration
Consider a 70-year-old male admitted with severe nausea, vomiting, and confusion who is diagnosed with acute hyponatremia (110 mEq/L) secondary to severe diarrhea. Intravenous hypertonic saline is initiated with close monitoring of serum sodium levels. The diarrhea is treated, and his sodium levels gradually normalize, with resolution of symptoms.
Important Note: This information is for educational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional for diagnosis and treatment of medical conditions.
Minimizing the Risk of Osmotic Demyelination Syndrome (ODS)
When treating hyponatremia, balancing the need for correction with the risk of complications is essential. Here’s how to minimize the risk of ODS:
- Gradual correction of low sodium levels is crucial to avoid ODS, aiming for increases of no more than 10 mEq/L/24 hours, and even less in high-risk patients. What alternative strategies exist for managing hyponatremia in patients at high risk for ODS?
- Carefully consider pre-existing conditions such as liver disease, alcohol use disorder, hypokalemia, and malnutrition, as these increase ODS risk.
- Closely monitor for neurological changes (e.g., confusion, dysarthria, dysphagia, weakness) throughout treatment.
- Collaborate with nephrology or endocrinology specialists to develop a coordinated treatment strategy.
Diagnosing Hyponatremia: Unraveling the Underlying Cause
Effective hyponatremia treatment starts with accurate diagnosis. Determining the etiology—hypovolemic, hypervolemic, or euvolemic—requires a comprehensive evaluation, including blood tests, a detailed medical history, and a thorough physical examination.
Treatment Strategies: A Meticulous Approach
Acute hyponatremia treatment requires gradual increases in serum sodium levels using hypertonic saline. Close monitoring of sodium levels and neurological status is
- Best Books on Meditation Recommended by Mindfulness Experts - January 30, 2026
- Best Mindfulness Books for Anxiety, Sleep, and Daily Peace - January 29, 2026
- Books On Mindfulness For A Happier, More Present Life - January 28, 2026