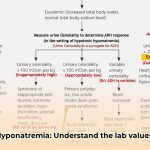
Low blood sodium (hyponatremia) is a common and potentially serious electrolyte disorder encountered in clinical practice. Correcting sodium levels safely requires a nuanced and individualized approach to avoid complications such as osmotic demyelination syndrome (ODS), a potentially devastating neurological condition. For more detailed guidelines, see the hyponatremia treatment guidelines. This comprehensive review article provides clinicians with an evidence-based guide to the safe and effective management of hyponatremia, covering acute and chronic presentations, common pitfalls, relevant treatment modalities, and a practical, step-by-step framework for clinical decision-making. Grounded in up-to-date research and established best practices, this guide aims to optimize patient outcomes and minimize iatrogenic risks.
Understanding the Importance of Safe Sodium Correction
Safely restoring serum sodium levels is of paramount importance for medical professionals managing patients with hyponatremia. The primary concern is the prevention of osmotic demyelination syndrome (ODS), a condition characterized by damage to the myelin sheath surrounding nerve cells in the brain, which can result in permanent neurological deficits. While prompt correction of hyponatremia is sometimes necessary, particularly in cases of acute, symptomatic hyponatremia, a slow and cautious approach is generally recommended, especially in chronic cases, to allow the brain to adapt to the changes in osmolality and prevent neurological complications.
The Rationale for a Gentle and Controlled Approach
Current clinical practice guidelines, supported by a wealth of clinical experience and observational studies, largely advocate for a gradual approach to correcting hyponatremia, particularly in patients with chronic hyponatremia. This approach aims to provide the brain with sufficient time to adapt to the changing serum sodium concentration, thereby mitigating the risk of ODS. However, emerging evidence suggests that a more nuanced and flexible approach may be appropriate in select patient populations. This evolving understanding underscores the need for clinicians to carefully evaluate each patient individually, taking into account the underlying cause of hyponatremia, the severity of symptoms, and the duration of the condition, and tailor treatment accordingly. Is a universally standardized approach truly optimal, or should treatment strategies be more adaptable to individual patient characteristics?
Differentiating Acute vs. Chronic Hyponatremia: A Guide to Tailored Management
Treatment strategies for hyponatremia depend significantly on whether the condition has developed acutely (within 48 hours) or chronically (over a period of days or weeks). Acute hyponatremia, particularly when accompanied by severe symptoms such as seizures or altered mental status, may necessitate more urgent initial intervention to prevent life-threatening complications. In contrast, chronic hyponatremia typically requires a slower correction rate, as the brain has had time to adapt to the reduced sodium levels, making it more vulnerable to rapid shifts in osmolality.
Individual Patient Assessment: Identifying Key Determinants of Treatment Strategy
Effective sodium correction necessitates a thorough and individualized patient assessment, with careful consideration of the following key factors:
- Severity of hyponatremia: The degree of sodium depletion is a critical determinant of the urgency and aggressiveness of the correction strategy.
- Presence and nature of symptoms: The presence of significant neurological symptoms, such as confusion, seizures, or coma, necessitates closer monitoring and potentially faster (but still cautious) correction.
- Etiology of hyponatremia: Identifying and addressing the underlying cause of hyponatremia is essential for long-term management and prevention of recurrence. Common etiologies include SIADH, diuretic use, renal disorders, and excessive water intake.
- Comorbidities: Coexisting medical conditions, such as heart failure, liver disease, and kidney disease, can significantly influence patient tolerance to sodium adjustments and increase the risk of complications.
- Patient age: Elderly individuals are often more susceptible to complications related to both hyponatremia and its treatment, requiring a more cautious approach.
- Volume status: Assessing the patient’s fluid status (hypovolemic, euvolemic, or hypervolemic) is crucial for guiding appropriate fluid management strategies.
Failure to adequately consider these elements can lead to adverse outcomes, including overcorrection, undercorrection, and ODS. To mitigate this risk, clinicians should adopt a standardized checklist or protocol to ensure that all relevant factors are systematically evaluated before initiating treatment.
Vigilant Monitoring: Detecting and Preventing Osmotic Demyelination Syndrome (ODS)
Close monitoring of serum sodium levels is paramount throughout the treatment process to ensure that the correction rate remains within safe limits. In addition to regular laboratory monitoring, frequent neurological assessments are essential for detecting early signs and symptoms of ODS, such as dysarthria, dysphagia, weakness, or altered mental status. While neuroimaging techniques such as MRI can be helpful in confirming the diagnosis of ODS, the interpretation of imaging studies can be challenging, and findings may not be evident in the early stages of the syndrome. Therefore, prompt recognition of clinical signs and symptoms is crucial for timely intervention and prevention of irreversible neurological damage. What non-invasive bedside methods can be used for routine neurological checks to detect subtle early indicators of ODS?
A Step-by-Step Framework for Safe Sodium Level Correction
The primary goal of hyponatremia treatment is to carefully restore serum sodium levels to a safe range while minimizing the risk of ODS and other complications. The following structured approach provides a framework for achieving this goal:
- Comprehensive Assessment: Obtain a detailed patient history, including the onset and duration of symptoms, the duration of hyponatremia (if known), and any potential underlying causes or contributing factors. Perform a thorough physical examination, paying particular attention to neurological and volume status.
- Etiological Diagnosis: Determine the underlying cause of the hyponatremia.
- Personalized Treatment Plan: Develop an individualized treatment plan based on the patient’s specific risk profile, including the severity of hyponatremia, the presence of symptoms, the underlying cause, and any comorbidities.
- Gradual Correction: Elevate serum sodium levels gradually, particularly in cases of chronic hyponatremia, adhering to recommended correction rates (typically no more than 4-8 mEq/L per 24 hours, and often lower in high-risk patients). Adjust the correction rate based on individual patient factors and response to treatment.
- Continuous Monitoring: Regularly assess serum sodium levels and neurological status, typically every 4-6 hours during the initial phase of treatment. Adjust the treatment plan as needed based on the patient’s response and laboratory values.
- Symptom Management: Address any accompanying symptoms, such as nausea, vomiting, or headache, with appropriate supportive care.
Effective communication and collaboration within the healthcare team are critical for ensuring patient safety and optimizing treatment outcomes. A study published in The New England Journal of Medicine demonstrated that implementing standardized communication protocols and checklists significantly reduced the incidence of medical errors and adverse events in hospitalized patients.
Future Directions: Addressing Knowledge Gaps and Improving Clinical Practice
Continued research is needed to further refine hyponatremia treatment guidelines, identify individuals at higher risk of complications, and develop more effective and targeted therapies. Collaborative efforts among clinicians, researchers, and regulatory agencies are crucial for advancing our understanding of hyponatremia and improving patient outcomes. Future research should prioritize the development of personalized treatment approaches that take into account the unique characteristics of each patient and the underlying pathophysiology of their condition.
Action Plan for Improved Hyponatremia Management
| Stakeholder | Immediate Actions | Long-Term Goals |
|---|---|---|
| Doctors and Nurses | Enhance monitoring protocols; improve staff training; standardize reporting; conduct thorough patient assessment. | Actively participate in research efforts to refine treatment protocols; promote continuous quality improvement initiatives. |
| Regulatory Agencies | Review and update existing guidelines; support collaborative research initiatives; disseminate evidence-based recommendations. | Fund research on innovative treatments and diagnostic tools; promote consistent standards; establish national benchmarks for hyponatremia management. |
| Pharmaceutical Industry | Develop safer sodium replacement therapies and advanced monitoring technologies; explore novel therapeutic targets. | Invest in research aimed at addressing underlying factors driving hyponatremia; develop personalized medicine approaches. |
Disclaimer: This information is intended for educational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional for any health concerns. Specific treatment decisions should be made in consultation with a qualified physician who can assess the individual patient’s condition and needs.
Managing Chronic Hyponatremia While Minimizing ODS Risk
Key Takeaways:
- Gradual sodium correction is vital to minimize the risk of osmotic demyelination syndrome (ODS).
- Treatment strategies should be tailored to the underlying cause, severity, and duration of hyponatremia.
- Regular monitoring of serum sodium levels and neurological status is essential.
- In specific cases, desmopressin can be used to prevent overcorrection and ODS.
- A multidisciplinary approach involving collaboration with healthcare professionals is critical for optimal management.
Understanding the Pathophysiology of Chronic Hyponatremia and Associated Risks
Chronic hyponatremia, characterized by a gradual decline in serum sodium levels over an extended period, presents unique management challenges. Rapid correction of chronic hyponatremia can significantly increase the risk of ODS, a potentially devastating neurological complication. As an analogy, consider repairing a bridge: rather than attempting repairs while traffic continues to flow, it’s essential to slow down and implement necessary precautions to ensure safety and stability.
Safe Sodium Level Correction: A Practical Approach
A gradual correction rate is paramount, with recommended increases typically not exceeding 4-6 mEq/L per 24 hours. Individualized treatment plans must consider the severity of hypon
- How Much Do Wellness Programs Cost Businesses To Offer? - December 16, 2025
- Wellness Fair Ideas for Work to Boost Employee Wellbeing - December 15, 2025
- Affordable Employee Wellness Fair Ideas for Any Budget - December 14, 2025