Hyponatremia, or low blood sodium, is a common and potentially serious condition. This guide explains hyponatremia, its diagnosis through lab values, and current management strategies. Whether you’re a healthcare professional or seeking to understand your own health, this resource will help you recognize, understand, and manage this condition effectively. For more on acute hyponatremia treatment, see this resource.
Hyponatremia: Unveiling Sodium Imbalance
Hyponatremia occurs when the sodium level in your blood drops below 135 mEq/L (milliequivalents per liter). Sodium is a key electrolyte that helps regulate fluid balance, nerve and muscle function. Understanding hyponatremia is crucial for timely intervention and preventing complications.
Sodium’s Vital Role in Fluid Balance
Sodium (Na+) is the major cation in the extracellular fluid, playing a critical role in maintaining osmotic pressure, nerve impulse transmission, and muscle contraction. It’s a key player in maintaining fluid balance and overall bodily functions.
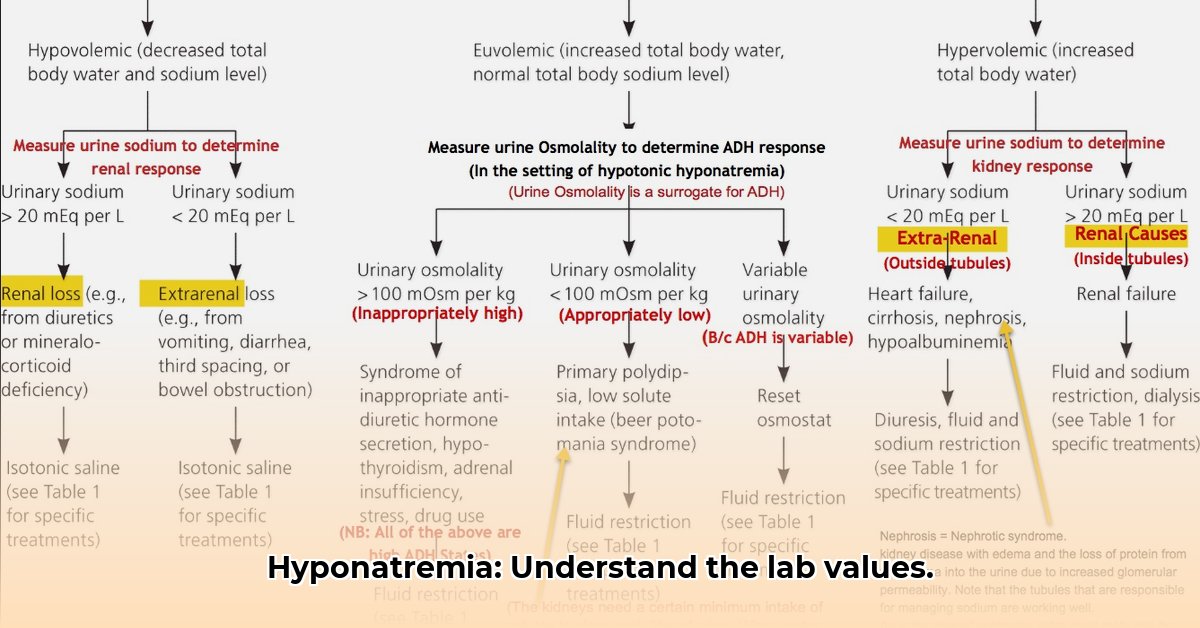
Diagnostic Tests and Evaluation: Interpreting Lab Results for Hyponatremia
Diagnosing hyponatremia requires a comprehensive evaluation that includes:
- Serum Sodium: A direct measurement of sodium concentration in your blood. A value below 135 mEq/L indicates hyponatremia.
- Serum Osmolality: Measures the concentration of dissolved particles in the blood. It helps distinguish true hyponatremia from pseudohyponatremia (where sodium levels are falsely low due to other substances in the blood). In true hyponatremia, serum osmolality is typically low (less than 275 mOsm/kg).
- Urine Osmolality: Assesses the kidney’s ability to concentrate or dilute urine. In hyponatremia, urine osmolality can help determine the underlying cause. A low urine osmolality (less than 100 mOsm/kg) suggests primary polydipsia (excessive water intake) or a low solute intake, while a high urine osmolality (greater than 100 mOsm/kg) indicates impaired water excretion.
- Urine Sodium: Measures the sodium concentration in the urine. It helps differentiate between different types of hyponatremia. A low urine sodium (less than 20 mEq/L) suggests volume depletion, while a high urine sodium (greater than 20-40 mEq/L) indicates SIADH or salt-wasting.
- Other Electrolytes: Measuring potassium, chloride, and bicarbonate levels can provide additional insights into the electrolyte balance and potential underlying causes of hyponatremia.
- Thyroid and Adrenal Function Tests: Thyroid-stimulating hormone (TSH) and cortisol levels are often checked to rule out hypothyroidism or adrenal insufficiency, which can contribute to hyponatremia.
Types of Hyponatremia
Hyponatremia is classified based on the patient’s volume status:
- Hypovolemic Hyponatremia: Occurs when both sodium and water are lost from the body, but sodium loss is greater. Causes include diarrhea, vomiting, diuretic use, and salt-wasting nephropathies. Urine sodium is usually low (less than 20 mEq/L) unless renal salt wasting is present.
- Euvolemic Hyponatremia: Characterized by a normal total body water but an excess of water relative to sodium. SIADH is the most common cause. Other causes include hypothyroidism, adrenal insufficiency, and certain medications. Urine sodium is typically high (greater than 20-40 mEq/L) in SIADH.
- Hypervolemic Hyponatremia: Occurs when there’s an increase in both sodium and water in the body, but the increase in water is proportionally greater. Common causes include heart failure, liver cirrhosis, and nephrotic syndrome. Urine sodium levels can vary depending on the underlying cause.
Risk Factors and Considerations Beyond Lab Results
A thorough medical history and physical examination are crucial for determining the cause of hyponatremia.
Important factors to consider include:
- Medication history (diuretics, antidepressants, etc.)
- Underlying medical conditions (heart failure, kidney disease, etc.)
- Dietary habits (low solute intake)
- Fluid intake (excessive water consumption)
- Symptoms (nausea, headache, confusion, seizures)
Personalized Management Strategies
Treatment for hyponatremia depends on the severity of the condition, the patient’s symptoms, and the underlying cause.
Treatment options include:
- Fluid Restriction: Limiting fluid intake is a primary strategy in euvolemic and hypervolemic hyponatremia.
- Sodium Supplementation: Administering oral or intravenous sodium to increase serum sodium levels.
- Diuretics: Loop diuretics can be used in hypervolemic hyponatremia to promote fluid excretion.
- Vasopressin Receptor Antagonists (Vaptans): These medications block the action of vasopressin, promoting water excretion without sodium loss.
- Treatment of Underlying Cause: Addressing the underlying medical condition (e.g., heart failure, SIADH) is crucial for long-term management of hyponatremia.
Care Coordination for Optimal Outcome
Managing hyponatremia requires a collaborative approach between healthcare providers, including physicians, nurses, and lab technicians. Proper interpretation of lab results, careful monitoring of sodium levels, and personalized treatment plans are essential for achieving the best possible outcome.
Safe Correction of Hyponatremia and Osmotic Demyelination Syndrome (ODS) Prevention
Key Takeaways:
- Rapid correction of chronic hyponatremia poses a significant risk of osmotic demyelination syndrome (ODS).
- Gradual correction is paramount to prevent neurological damage and long-term complications.
- Individualized treatment plans, considering factors such as initial sodium levels, comorbidities, and underlying causes, are essential.
The Link Between Hyponatremia and ODS Risk
Hyponatremia can lead to osmotic shifts in brain cells. If sodium levels are corrected too quickly, it can cause cellular damage and ODS.
Gradual Hyponatremia Correction: Essential for Neurological Safety
The primary principle is to correct sodium levels gradually:
- The general guideline is to limit the increase in serum sodium to ≤10 mEq/L in the first 24 hours and ≤8 mEq/L per 24 hours subsequently.
- In patients with severe hyponatremia (<115 mEq/L) or those at high risk for ODS, a slower correction rate of ≤6 mEq/L per 24 hours is recommended.
Individualized Treatment: A Tailored Approach
Individualized treatment plans are essential for safe correction. Key factors include:
- Severity of hyponatremia
- Duration of hyponatremia (acute vs. chronic)
- Underlying cause of hyponatremia
- Patient’s overall health and comorbidities
- Risk factors for ODS (alcoholism, liver disease, malnutrition)
Vigilance and Early Intervention: Monitoring and Prevention
Continuous monitoring of serum sodium levels is essential during treatment. Regular blood tests are crucial to track the correction rate and adjust the treatment plan accordingly. Be alert for neurological symptoms that suggest ODS, such as:
- Confusion
- Lethargy
- Dysarthria (difficulty speaking)
- Dysphagia (difficulty swallowing)
- Quadriparesis (weakness in all four limbs)
Fluid Management and Hypertonic Saline
Hypertonic saline (3% NaCl) is often used to treat severe, symptomatic hyponatremia. However, it must be administered cautiously to avoid overcorrection. It’s important to calculate the sodium deficit and administer the hypertonic saline slowly, with frequent monitoring of serum sodium levels.
Addressing the Underlying Medical Causes
In addition to correcting the sodium level, it’s crucial to identify and treat the underlying cause of hyponatremia. This may involve:
- Discontinuing offending medications (e.g., diuretics, SSRIs)
- Treating underlying medical conditions (e.g., heart failure, SIADH)
- Managing fluid balance
- Providing nutritional support
The Importance of Supportive Care
Supportive care is also important for patients with hyponatremia. This may include:
- Thiamine supplementation (especially in patients with alcoholism or malnutrition)
- Nutritional support
- Physical therapy
- Occupational therapy
[UpToDate: Osmotic demyelination syndrome (ODS) and overly rapid correction of hyponatremia]
- How Much Do Wellness Programs Cost Businesses To Offer? - December 16, 2025
- Wellness Fair Ideas for Work to Boost Employee Wellbeing - December 15, 2025
- Affordable Employee Wellness Fair Ideas for Any Budget - December 14, 2025